Introduction
This article explores the anatomy and physiology of human reproduction. It highlights key structures and processes in female and male reproductive systems, and explains how hormonal and physiological changes support fertility, pregnancy, childbirth, and lactation.
Contents
Female Reproductive Anatomy
External Genitalia
The external female genital structures are collectively known as the vulva. Key components include:
- Mons Pubis: A fatty pad over the pubic bone that becomes covered with hair during puberty.
- Labia Majora: The larger, outer lips extending from the mons pubis to the perineum, containing sweat and sebaceous glands, and hair follicles. They protect the inner genital structures.
- Labia Minora: The smaller, inner lips are located within the labia majora, extending from the clitoris to the fourchette. They are highly vascularized, hairless, and rich in nerve endings.
- Clitoris: A highly sensitive erectile organ at the anterior junction of the labia minora. It contains about 8,000 sensory nerve endings and is homologous1 to the penis. The visible glans is only part of the internal clitoral structure.
- Vestibule: The space enclosed by the labia minora, containing the urethral opening and vaginal introitus.
- Bartholin’s Glands: Two small glands near the vaginal opening that secrete lubricating fluid during sexual arousal.
- Perineum: The area between the vaginal opening and the anus, composed of muscle, connective tissue, and the perineal body, which supports the pelvic floor.
Internal Reproductive Organs
- Vagina: A muscular, elastic canal (approximately 7.5–10 cm long) with a mucosal lining. It connects the external genitalia to the uterus, accommodates childbirth, and maintains an acidic pH (± 3.8–4.5) through lactobacilli to inhibit pathogens.2
- Uterus: A hollow, pear-shaped muscular organ (±7.5 cm long, 5 cm wide, 2.5 cm thick in a non-pregnant state) where a fertilised ovum implants and develops. Key parts include:
- Fundus: The rounded top above the fallopian tube openings.
- Corpus (Body): The main central portion.
- Isthmus: The narrowed segment between the corpus and cervix.
- Cervix: The lower cylindrical section projecting into the vagina; it connects to the vagina via the external os and to the uterine cavity via the internal os.
- Uterine Wall Layers:
- Perimetrium: The outer serous membrane.
- Myometrium: The thick middle muscular layer responsible for uterine contractions during labour.
- Endometrium: The inner mucosal layer that thickens and sheds in response to hormonal cycles.
- Cervix: The cervical canal contains glands that produce mucus. The consistency of cervical mucus changes throughout the menstrual cycle (becoming thinner and more stretchable around ovulation), which helps facilitate sperm entry during fertile days.
- Fallopian Tubes (Uterine Tubes): Two tubes (10–12 cm long) extending from the uterus toward the ovaries. They transport the ova and are typically where fertilisation occurs. Segments include:
- Interstitial (Intramural) Segment: The portion that passes through the uterine wall.
- Isthmus: A narrow, straight segment.
- Ampulla: A wider, curved segment where fertilisation usually takes place.
- Infundibulum: The funnel-shaped end near the ovary, with fimbriae that sweep over the ovary to capture the ovulated egg.
- Ovaries: Paired almond-shaped glands (± 3–5 cm long) that produce ova (eggs) and sex hormones (estrogen and progesterone). Each ovary contains roughly 1–2 million primordial3 follicles at birth; only about 300–400 ova are released during a typical female reproductive lifetime.
Pelvic Floor
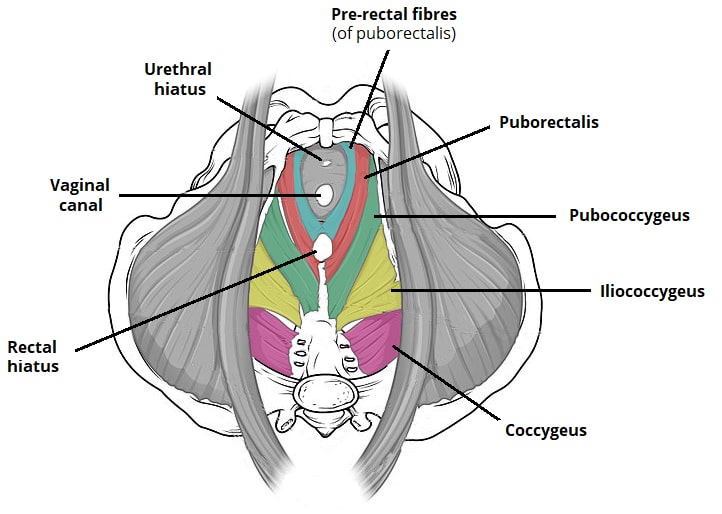
The pelvic floor consists of muscles and connective tissues that support the pelvic organs. Important components are:
- Levator Ani Complex: The primary muscle group (including pubococcygeus, iliococcygeus, and puborectalis) forms a supportive sling for the pelvic viscera.
- Coccygeus (Ischiococcygeus): A smaller muscle that works with the levator ani.
- Perineal Muscles: Including bulbospongiosus, ischiocavernosus, and transverse perineal muscles, reinforcing pelvic floor support.
- Pelvic Fascia: A connective tissue layer that adds structural support.
A strong pelvic floor is essential for normal childbirth mechanics and for preventing pelvic organ prolapse or incontinence.
Male Reproductive Anatomy
Key male reproductive structures include:
- Testes: Paired oval glands in the scrotum that produce sperm and testosterone. Their location outside the body keeps them at a cooler temperature, optimal for sperm production.
- Epididymis: A coiled duct on the surface of each testis where sperm mature and gain motility after leaving the testis.
- Vas Deferens: The muscular tube that transports sperm from the epididymis into the ejaculatory ducts during ejaculation.
- Seminal Vesicles: Glands that secrete a fructose-rich fluid (about 70% of semen) to nourish and transport sperm.
- Prostate Gland: Produces an alkaline fluid (prostate fluid) that neutralises the acidity of vaginal secretions, enhancing sperm survival.
- Penis: The external organ composed of erectile tissue. During sexual arousal, the corpora cavernosa and corpus spongiosum become engorged with blood, leading to erection. The glans is the sensitive tip, which in uncircumcised males is covered by the foreskin (prepuce).
- Urethra: The dual-purpose canal that carries both urine (from the bladder) and semen (from the ejaculatory ducts) to the outside of the body.
Physiology of the Menstrual Cycle
The menstrual cycle is a roughly monthly cycle that prepares the body for potential pregnancy. It involves coordinated hormone signalling between the brain and the ovaries:
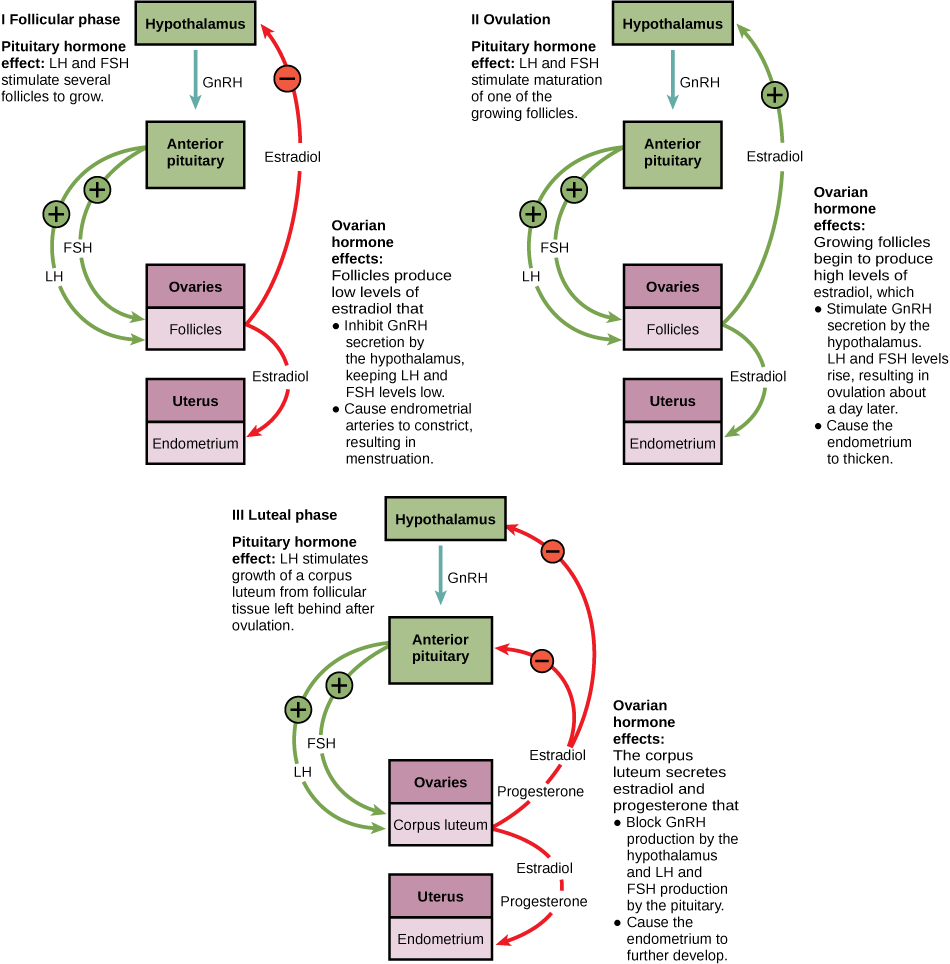
Hormonal Regulation
- The hypothalamus secretes gonadotropin-releasing hormone (GnRH) in pulses.
- GnRH stimulates the anterior pituitary to release follicle-stimulating hormone (FSH) and luteinizing hormone (LH).
- FSH promotes the growth of ovarian follicles. The developing follicles produce estrogen.
- Rising estrogen eventually triggers a surge of LH, causing ovulation (the release of a mature ovum).
- After ovulation, the ruptured follicle becomes the corpus luteum, which secretes progesterone (and some estrogen). Progesterone prepares the endometrium for possible embryo implantation.
- Estrogen and progesterone exert feedback on the hypothalamus and pituitary to regulate further GnRH, FSH, and LH release.
Ovarian Cycle (Ovarian Phases)
- Follicular Phase (Day 1–13): Begins on the first day of menstruation. Rising FSH stimulates several follicles to develop; these follicles produce estrogen. Usually, one follicle becomes dominant while the others regress.
- Ovulation (Day 14 approximate): An LH surge causes the dominant follicle to rupture, releasing the ovum into the fallopian tube.
- Luteal Phase (Day 15–28): The remaining follicle tissue transforms into the corpus luteum, secreting progesterone (and some estrogen). If pregnancy does not occur, the corpus luteum degenerates after about 10–14 days, progesterone levels fall, and menstruation ensues.
Endometrial Cycle (Uterine Phases)
- Menstrual Phase (Day 1–5): The functional layer of the endometrium is shed, resulting in menstrual bleeding (typically 30–80 mL of blood loss).
- Proliferative Phase (Day 6–14): Under estrogen influence, the endometrium regenerates and thickens (from ~0.5 mm to 3.5–5 mm by ovulation), with lengthening glands and development of blood vessels.
- Secretory Phase (Day 15–28): After ovulation, progesterone causes the endometrium to become secretory. Glands secrete nutrients, vascularisation increases, and the lining reaches its maximum thickness (5–7 mm) to support embryo implantation. If no implantation occurs, progesterone drops and menstruation begins.
Physiology of Fertilisation and Early Development
Fertilisation
- Sperm Transport: At ejaculation, 200–500 million sperm are deposited into the vagina. Sperm travel through the cervical canal (which is most receptive around ovulation) and enter the uterus. They undergo capacitation (a functional maturation in the female tract). Only a few thousand sperm reach the ampulla of the fallopian tube.
- Fertilisation Process: Usually occurs in the ampulla. A single sperm penetrates the ovum’s zona pellucida, triggering a cortical reaction that prevents other sperm from entering (blocking polyspermy). The sperm nucleus then fuses with the ovum nucleus to form a diploid zygote, combining genetic material from both parents.
Early Embryonic Development
- Cleavage: The zygote undergoes rapid mitotic divisions without growing in size. These produce smaller cells called blastomeres. By around Day 3, a solid ball of 12–16 cells called the morula has formed.
- Blastocyst Formation (Days 4–5): A fluid-filled cavity (blastocoel) appears within the morula, forming a blastocyst. Cells differentiate into the trophoblast (outer layer, which will form the placenta and fetal membranes) and the inner cell mass (which will become the embryo).
- Implantation (Days 6–12): The blastocyst attaches to and invades the endometrium (usually on the upper posterior uterine wall). Trophoblastic cells penetrate the endometrium, establishing early maternal-fetal circulation. The developing trophoblast secretes human chorionic gonadotropin (hCG), which signals the corpus luteum to continue producing progesterone.
Early Placental Development
- Trophoblast Differentiation: The trophoblast forms two layers: the cytotrophoblast (inner cellular layer) and the syncytiotrophoblast (outer layer that invades maternal tissue).
- Chorionic Villi Formation: Finger-like projections of trophoblast form villi: primary villi (syncytiotrophoblast outgrowths), secondary villi (with a core of cytotrophoblast), and tertiary villi (with fetal blood vessels in the core).
- Placental Circulation: Maternal blood flows into the intervillous spaces of the placenta. Fetal blood circulates through vessels in the chorionic villi. By about week 12, maternal and fetal blood supplies are connected via the placenta, allowing efficient nutrient and gas exchange.
Physiological Adaptations to Pregnancy
Pregnancy induces significant changes in nearly every maternal body system to support the growing fetus:
Reproductive System Changes
- Uterus: Dramatic enlargement (from ±70 g to ±1100 g by term; volume increases ±500-fold). Myometrial fibres hypertrophy, and uterine blood flow increases from ±50 mL/min (nonpregnant) to 500–700 mL/min at term.
- Cervix: Increased blood flow causes a bluish colouration (Chadwick’s sign). The cervix softens (Goodell’s sign) as collagen remodels and water content rises. A thick mucus plug forms to seal the uterus.
- Vagina: Becomes more vascular and elastic. The mucosa thickens and secretions increase (leukorrhea) with a more acidic pH (±3.5–6.0) to protect against infection.
- Ovaries: Ovulation ceases. The corpus luteum (from the last ovulation) continues to produce progesterone until the placenta takes over (±10–12 weeks). Ovaries also produce relaxin, which helps relax pelvic ligaments and soften the cervix.
Cardiovascular Changes
- Blood Volume: Increases by ±40–45% (about +1500 mL) by term. Plasma volume expands more than red cell mass, leading to physiological anaemia of pregnancy.
- Cardiac Output: Rises by ±30–50% by mid-pregnancy. Heart rate increases by ±10–15 beats per minute, and stroke volume increases, meeting the higher metabolic demands.
- Blood Pressure: Systemic vascular resistance decreases (due to progesterone and placental hormones), often causing a drop in blood pressure during the first and second trimesters. It usually returns toward baseline by the term.
- Venous Changes: The enlarging uterus can compress pelvic veins and the inferior vena cava, causing venous stasis in the legs. This increases the risk of varicose veins and deep vein thrombosis.
Respiratory System
- Anatomical Changes: The diaphragm elevates by up to 4 cm as the uterus enlarges, and the chest expands (thoracic circumference increases by 5–7 cm). The subcostal angle widens.
- Pulmonary Function: Tidal volume (air per breath) increases by ±30–40%. Minute ventilation (air per minute) increases ±40%, resulting in a mild respiratory alkalosis (lower CO₂ levels). Residual lung volumes decrease slightly.
- Oxygen Consumption: Maternal oxygen use increases by ±20–30% by term to meet both maternal and fetal metabolic needs.
Renal System
- Structural Changes: Renal pelvis and ureters dilate (especially the right ureter). Kidneys enlarge (±1–1.5 cm increase in length).
- Functional Changes: Glomerular filtration rate (GFR) and renal plasma flow increase by ±50%. This can lead to increased clearance of substances and sometimes mild glycosuria. Bladder capacity increases, although frequent urination is common due to pressure on the bladder.
Gastrointestinal System
- Mechanical Effects: The growing uterus displaces the stomach and intestines upward. Gastric emptying slows, and intestinal motility4 decreases (progesterone effect), which can cause constipation and increase reflux (heartburn).
- Functional Changes: Nausea and vomiting (morning sickness5) are common, especially in the first trimester. Nutrient and vitamin requirements increase to support fetal growth. Liver metabolism changes (e.g., increased cholesterol production for steroidogenesis).
Endocrine System
- Placental Hormones: The placenta produces large amounts of estrogen, progesterone, human chorionic gonadotropin (hCG), human placental lactogen (hPL), relaxin, and others (activin, inhibin).
- Pituitary Changes: The anterior pituitary enlarges. Prolactin levels rise steadily to prepare the breasts, although high estrogen and progesterone during pregnancy inhibit milk production until after birth. Near term, the posterior pituitary increases oxytocin storage for labour.
- Thyroid: Thyroid-binding globulin levels increase (due to high estrogen), raising total thyroid hormones. Basal metabolic rate increases (±20%). Pregnancy causes a slight physiological hyperthyroxinemia, usually without thyroid disease.
Metabolic Adaptations
- Weight Gain: Recommended gain is ±11–16 kg (25–35 lbs) for normal-weight women. This includes the fetus (3–4 kg), placenta (0.5–0.7 kg), amniotic fluid (0.8–1.2 kg), enlarged uterus (0.9–1.2 kg), increased blood volume (1.2–1.5 kg), enlarged breasts (0.9–1.5 kg), and maternal fat stores (3–4 kg).
- Glucose Metabolism: Pregnancy induces insulin resistance (due to placental hormones like hPL6), so maternal insulin production increases. This ensures sufficient glucose is available to the fetus (often called a mild diabetogenic state).
- Nutrient Storage: Women enter a state of positive nitrogen balance; protein synthesis and nutrient storage increase to support fetal growth. An extra ±300 kilocalories per day (especially in the third trimester) is generally recommended to meet fetal and maternal demands.
Physiology of Labour and Birth
Initiation of Labour (Parturition)
The exact trigger for labour involves multiple factors:
- Hormonal Changes: A relative decrease in progesterone activity (despite high progesterone levels) and a relative increase in estrogen action prime the uterus for contractions. Estrogen increases oxytocin receptor and prostaglandin receptor expression in the myometrium.
- Oxytocin: Maternal oxytocin levels rise near term, and the uterus becomes more sensitive to it. Oxytocin stimulates uterine contractions.
- Prostaglandins: Prostaglandins (especially PGE2 and PGF2α) increase in fetal membranes and amniotic fluid, promoting cervical ripening (softening and dilation) and stimulating uterine contractions.
- Fetal Signals: The maturing fetus contributes signals: a surge of fetal cortisol increases placental corticotropin-releasing hormone (CRH), which may enhance uterine readiness. Fetal lung maturation and surfactant proteins may also play a role in triggering labour.
Prelabor Changes
- Cervical Ripening: The cervix softens and dilates as collagen is broken down and water content increases. Hyaluronic acid and glycosaminoglycans increase between collagen fibres, allowing them to separate.
- Uterine Sensitisation: Myometrial cells develop more gap junctions (fused channels) for synchronised contractions. Oxytocin7 receptor density in the myometrium increases.
- Braxton Hicks Contractions: These are irregular, usually painless uterine contractions that may increase in frequency as term approaches, but they do not cause cervical dilation.
Stages of Labour
- First Stage: From true labour onset to full cervical dilation (10 cm). It includes:
- Latent Phase: Slow effacement (thinning) and dilation of the cervix (up to ~3 cm).
- Active Phase: More rapid cervical dilation (about 4–7 cm).
- Transition Phase: Final dilation from 8 to 10 cm (often the most intense contractions).
- Second Stage: From full dilation to birth of the baby. The fetus descends through the birth canal, rotates, and is expelled by maternal effort.
- Third Stage: From delivery of the baby to delivery of the placenta. After the baby is born, continued uterine contractions detach the placenta from the uterus, which is then delivered.
- Fourth Stage: The first few hours after delivery, during which the mother’s uterus contracts to control bleeding (postpartum hemostasis) and initial mother-infant bonding and breastfeeding begin.
Lactation Physiology
Mammary Gland Development
- Embryonic: Mammary ridges form at 4–6 weeks of embryonic development, establishing the rudimentary ductal system by birth.
- Puberty: Estrogen stimulates ductal growth; progesterone promotes lobuloalveolar (milk gland) development. Fat deposition shapes the adult breast contour.
- Pregnancy: Elevated levels of estrogen, progesterone, prolactin, and human placental lactogen lead to extensive lobular and alveolar growth, increased vascularity, and the development of secretory cells. Colostrum (early antibody-rich milk) can be produced by mid-pregnancy, though high progesterone prevents secretion until after birth.
Hormonal Control of Lactation
- During Pregnancy, High levels of estrogen and progesterone stimulate breast development. Prolactin levels rise, but do not induce lactation due to progesterone’s inhibitory effect.
- After Birth, the delivery of the placenta causes estrogen and progesterone levels to drop sharply. This removes inhibition, allowing prolactin (which is now high) to initiate milk production (lactogenesis).
- Oxytocin and Milk Ejection: Suckling by the infant stimulates the release of oxytocin from the posterior pituitary, causing myoepithelial cells around the alveoli to contract and eject milk into the ducts (“let-down” reflex).
- Supply and Demand: Frequent milk removal (by nursing or pumping) sustains milk production via a feedback mechanism. If the breasts are not regularly emptied, a local inhibitor (Feedback Inhibitor of Lactation) accumulates and gradually reduces milk synthesis.
Milk Production Stages
- Colostrum (Days 1–3 postpartum): A thick, yellowish fluid high in protein (especially immunoglobulins) and minerals, with a mild laxative effect to help clear the newborn’s intestines. It is relatively low in fat and lactose.
- Transitional Milk (Days 3–5): Colostrum gradually transitions to mature milk; volume increases, and fat and lactose content rise.
- Mature Milk (From Day 5–7 onward): Composed of:
- Foremilk: The initial milk during a feeding, which is thinner and higher in lactose (hydration).
- Hindmilk: Comes later in the feeding and is higher in fat (energy-dense).
The composition of mature milk can adjust over time to meet the nutritional needs of the growing infant.
Conclusion
A thorough understanding of reproductive anatomy and physiology is essential for midwives and healthcare providers. It forms the foundation for recognising normal versus abnormal patterns and guiding evidence-based care throughout conception, pregnancy, childbirth, and the postpartum period. Mastery of these fundamentals supports the health of both mother and infant at every stage of the reproductive journey.
Elaborations.
- Similarity in anatomical structures ↩︎
- Pathogens are microorganisms that have the potential to cause infectious diseases. Viruses, bacteria, protozoans and fungi are all potential pathogens. A pathogen is defined as an organism that has the potential to cause infectious diseases in its host. ↩︎
- (of a cell, part, or tissue) In the earliest stage of development. ↩︎
- The ability of an organism to move independently, using metabolic energy ↩︎
- Hyperemesigravidarum ↩︎
- Human placental lactogen (hPL), previously known as human chorionic somatomammotropin, is a polypeptide hormone produced during pregnancy by the syncytiotrophoblast cells of the placenta. ↩︎
- Oxytocin is a natural hormone made in the brain. It is stored and released into the bloodstream by the pituitary gland. Oxytocin plays a key role in both the female and male reproductive systems. This includes increasing contractions to induce labour and birth, and the release of milk from the breast after birth. ↩︎
- Citations
Tailored Prenatal Care Delivery for Pregnant Individuals | ACOG
https://www.acog.org/clinical/clinical-guidance/clinical-consensus/articles/2025/04/tailored-prenatal-care-delivery-for-pregnant-individuals
New guidelines on antenatal care for a positive pregnancy experience
https://www.who.int/news/item/07-11-2016-new-guidelines-on-antenatal-care-for-a-positive-pregnancy-experience
New guidelines on antenatal care for a positive pregnancy experience
https://www.who.int/news/item/07-11-2016-new-guidelines-on-antenatal-care-for-a-positive-pregnancy-experience
Recommendations | Antenatal care | Guidance | NICE
https://www.nice.org.uk/guidance/ng201/chapter/Recommendations
New guidelines on antenatal care for a positive pregnancy experience
https://www.who.int/news/item/07-11-2016-new-guidelines-on-antenatal-care-for-a-positive-pregnancy-experience
New guidelines on antenatal care for a positive pregnancy experience
https://www.who.int/news/item/07-11-2016-new-guidelines-on-antenatal-care-for-a-positive-pregnancy-experience
Evaluation of the Obstetric Patient – Gynecology and Obstetrics – Merck Manual Professional Edition
https://www.merckmanuals.com/professional/gynecology-and-obstetrics/approach-to-the-pregnant-woman-and-prenatal-care/evaluation-of-the-obstetric-patient
Your antenatal care – NHS
https://www.nhs.uk/pregnancy/your-pregnancy-care/your-antenatal-care/
Evaluation of the Obstetric Patient – Gynecology and Obstetrics – Merck Manual Professional Edition
https://www.merckmanuals.com/professional/gynecology-and-obstetrics/approach-to-the-pregnant-woman-and-prenatal-care/evaluation-of-the-obstetric-patient
Your antenatal care – NHS
https://www.nhs.uk/pregnancy/your-pregnancy-care/your-antenatal-care/
Evaluation of the Obstetric Patient – Gynecology and Obstetrics – Merck Manual Professional Edition
https://www.merckmanuals.com/professional/gynecology-and-obstetrics/approach-to-the-pregnant-woman-and-prenatal-care/evaluation-of-the-obstetric-patient
Patient Screening | ACOG
https://www.acog.org/programs/perinatal-mental-health/patient-screening
Update on Prenatal Care | AAFP
https://www.aafp.org/pubs/afp/issues/2014/0201/p199.html
Update on Prenatal Care | AAFP
https://www.aafp.org/pubs/afp/issues/2014/0201/p199.html
Evaluation of the Obstetric Patient – Gynecology and Obstetrics – Merck Manual Professional Edition
https://www.merckmanuals.com/professional/gynecology-and-obstetrics/approach-to-the-pregnant-woman-and-prenatal-care/evaluation-of-the-obstetric-patient
Update on Prenatal Care | AAFP
https://www.aafp.org/pubs/afp/issues/2014/0201/p199.html
Evaluation of the Obstetric Patient – Gynecology and Obstetrics – Merck Manual Professional Edition
https://www.merckmanuals.com/professional/gynecology-and-obstetrics/approach-to-the-pregnant-woman-and-prenatal-care/evaluation-of-the-obstetric-patient
Update on Prenatal Care | AAFP
https://www.aafp.org/pubs/afp/issues/2014/0201/p199.html
Update on Prenatal Care | AAFP
https://www.aafp.org/pubs/afp/issues/2014/0201/p199.html
Routine Tests During Pregnancy | ACOG
https://www.acog.org/womens-health/faqs/routine-tests-during-pregnancy
Prenatal Panel: MedlinePlus Medical Test
https://medlineplus.gov/lab-tests/prenatal-panel/
Prenatal Panel: MedlinePlus Medical Test
https://medlineplus.gov/lab-tests/prenatal-panel/
Prenatal Panel: MedlinePlus Medical Test
https://medlineplus.gov/lab-tests/prenatal-panel/
Your antenatal care – NHS
https://www.nhs.uk/pregnancy/your-pregnancy-care/your-antenatal-care/
Update on Prenatal Care | AAFP
https://www.aafp.org/pubs/afp/issues/2014/0201/p199.html
Update on Prenatal Care | AAFP
https://www.aafp.org/pubs/afp/issues/2014/0201/p199.html
Recommendations | Antenatal care | Guidance | NICE
https://www.nice.org.uk/guidance/ng201/chapter/Recommendations
Update on Prenatal Care | AAFP
https://www.aafp.org/pubs/afp/issues/2014/0201/p199.html
Update on Prenatal Care | AAFP
https://www.aafp.org/pubs/afp/issues/2014/0201/p199.html
Update on Prenatal Care | AAFP
https://www.aafp.org/pubs/afp/issues/2014/0201/p199.html
Weight Gain During Pregnancy | Maternal Infant Health | CDC
https://www.cdc.gov/maternal-infant-health/pregnancy-weight/index.html
Update on Prenatal Care | AAFP
https://www.aafp.org/pubs/afp/issues/2014/0201/p199.html
Update on Prenatal Care | AAFP
https://www.aafp.org/pubs/afp/issues/2014/0201/p199.html
Update on Prenatal Care | AAFP
https://www.aafp.org/pubs/afp/issues/2014/0201/p199.html
New guidelines on antenatal care for a positive pregnancy experience
https://www.who.int/news/item/07-11-2016-new-guidelines-on-antenatal-care-for-a-positive-pregnancy-experience
Recommendations | Antenatal care | Guidance | NICE
https://www.nice.org.uk/guidance/ng201/chapter/Recommendations
Recommendations | Antenatal care | Guidance | NICE
https://www.nice.org.uk/guidance/ng201/chapter/Recommendations
Recommendations | Antenatal care | Guidance | NICE
https://www.nice.org.uk/guidance/ng201/chapter/Recommendations
Recommendations | Antenatal care | Guidance | NICE
https://www.nice.org.uk/guidance/ng201/chapter/Recommendations
Recommendations | Antenatal care | Guidance | NICE
https://www.nice.org.uk/guidance/ng201/chapter/Recommendations
Recommendations | Antenatal care | Guidance | NICE
https://www.nice.org.uk/guidance/ng201/chapter/Recommendations
Update on Prenatal Care | AAFP
https://www.aafp.org/pubs/afp/issues/2014/0201/p199.html



